There could be new hope for millions of patients suffering from Alzheimer’s disease with the US Food and Drug Administration (FDA) approving Leqembi, a drug that has shown it can slow down cognitive decline, but also comes with potential safety risks.
Leqembi, (lecanemab-irmb) is the second of a new category of medications approved for Alzheimer’s disease that target the fundamental pathophysiology of the disease, instead of just the symptoms. FDA said, “these medications represent an important advancement in the ongoing fight to effectively treat Alzheimer’s disease”.
Alzheimer’s disease – an irreversible, progressive brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out simple tasks – makes up for 60 to 70 percent of all dementia cases worldwide. A World Health Organisation (WHO) report in 2021 said the number of people living with dementia is set to rise to 139 million by 2050, compared to the 55 million people who have it now.
The drug has been developed by the Tokyo-based Eisai and American Biogen and will be commercially available by January 23. Eisai estimates that the drug delayed patients’ disease getting worse by about five months over 18 months of treatment.
According to an Associated Press report, the drug will cost $26,500 for a typical year’s worth of treatment. Eisai said that price reflects the drug’s benefit in terms of improved quality of life, reduced burdens for caregivers and other factors, and that it priced the drug lower to reduce costs for patients and insurers. However, an independent group that assesses drug value said that it would have to be priced below $20,600 to be cost-effective.
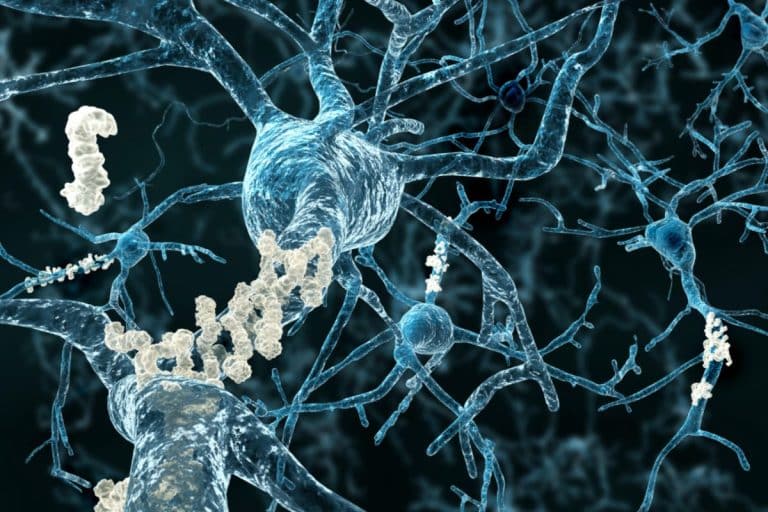
Following Phase 3 clinical trials, the companies said that lecanemab – an antibody designed to remove sticky deposits of a protein called amyloid beta on brain neurons and their connections – reduced the rate of cognitive decline on a clinical dementia scale (CDR-SB) by 27 percent compared to the placebo.
A similar anti-amyloid drug from Eli Lilly is also up for early approval sometime soon.
However, it also led to two deaths during the trials, and is associated with risks of swelling and bleeding in the brain. Eisai had said the deaths were caused because the two patients were on blood-thinning medication.
Leqembi was approved using the Accelerated Approval pathway, under which the FDA may approve drugs for serious conditions where there is an unmet medical need and a drug is shown to have an effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients.
Billy Dunn, MD, director of the Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said: “Alzheimer’s disease immeasurably incapacitates the lives of those who suffer from it and has devastating effects on their loved ones. This treatment option is the latest therapy to target and affect the underlying disease process of Alzheimer’s, instead of only treating the symptoms.”

FDA said the prescribing information for Leqembi includes a warning for amyloid-related imaging abnormalities (ARIA), which are known to occur with antibodies of this class. ARIA most commonly presents as temporary swelling in areas of the brain that usually resolves over time and may be accompanied by small spots of bleeding in or on the surface of the brain, though some people may have symptoms such as headache, confusion, dizziness, vision changes, nausea and seizure.